Understanding the Warning Signs of Congestive Heart Failure: What to Look For
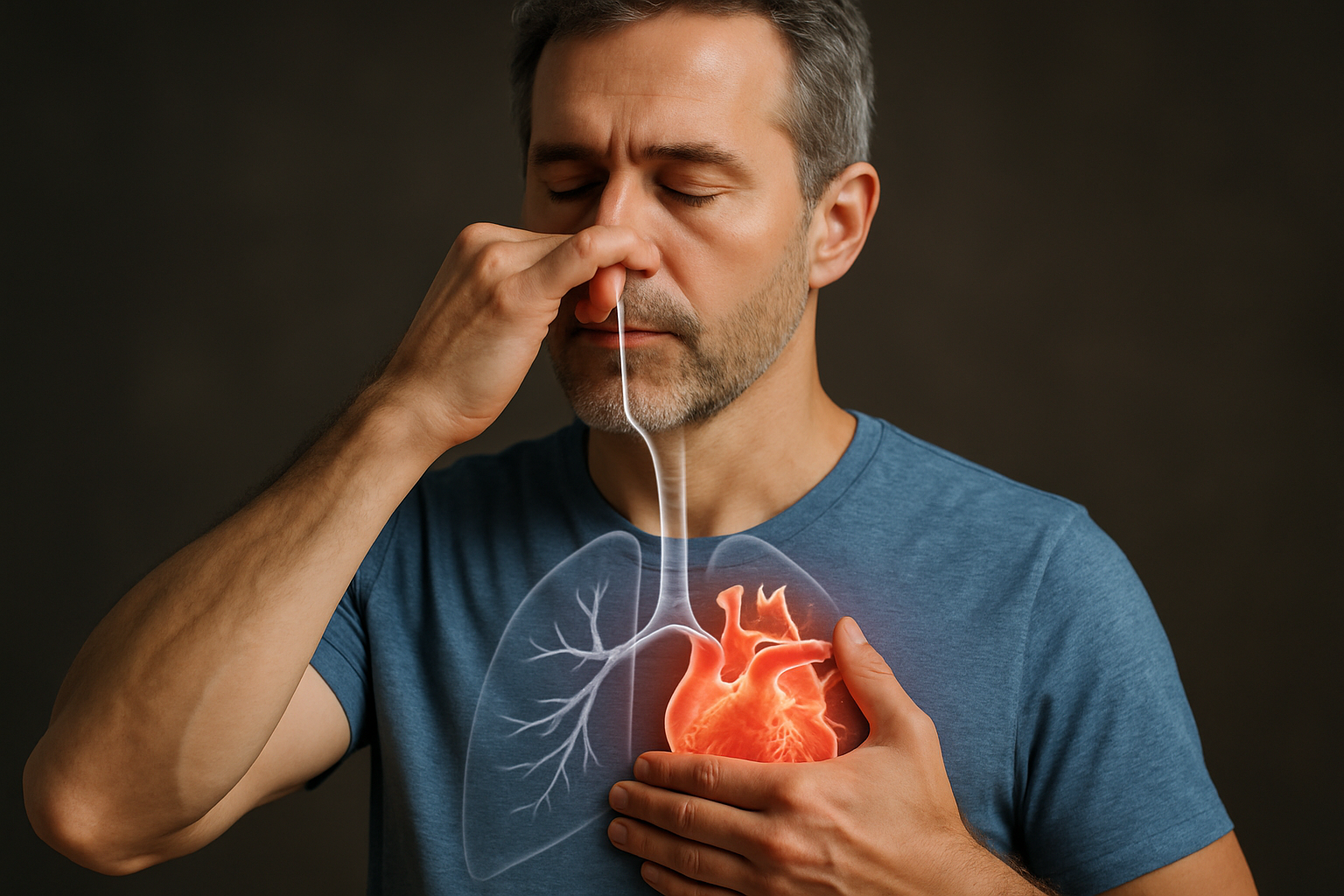
Congestive heart failure develops gradually, and early recognition is important for seeking timely care. This article explains the early signs of congestive heart failure, how symptoms may progress, why warning signs are often missed, and when to consult a doctor for evaluation.
What Are the Early Signs of Congestive Heart Failure?
The initial symptoms of congestive heart failure can be subtle and easily overlooked. Fatigue that seems disproportionate to your activity level is often one of the earliest signs. You might feel unusually tired after routine activities that never bothered you before. Shortness of breath, particularly during physical activity or when lying down flat in bed, is another common early indicator. Many patients report needing to prop themselves up with pillows to breathe comfortably while sleeping, a condition known as orthopnea.
Swelling (edema) in the feet, ankles, and legs occurs as fluid backs up in the body due to poor circulation. This swelling typically worsens throughout the day and may improve overnight when legs are elevated. Weight gain that happens rapidly—two to three pounds in a day or five pounds in a week—can indicate fluid retention related to heart failure. A persistent cough, especially one that produces white or pink-tinged mucus, might develop as fluid builds up in the lungs.
How Do Symptoms of Congestive Heart Failure Progress Over Time?
As heart failure advances, symptoms typically become more pronounced and difficult to ignore. What begins as shortness of breath during exercise may progress to breathlessness even at rest. Fatigue becomes more severe, significantly limiting daily activities and independence. Fluid retention increases, with swelling potentially spreading from the lower extremities to the abdomen (a condition called ascites).
Heart rhythm irregularities may develop or worsen, causing palpitations or a sensation of skipped or racing heartbeats. Mental symptoms emerge as reduced cardiac output affects brain function—confusion, impaired memory, and difficulty concentrating can result. Sleep disturbances become common, including sleep apnea and paroxysmal nocturnal dyspnea (sudden awakening with severe shortness of breath).
In advanced stages, symptoms can become debilitating. Patients may experience cyanosis (bluish discoloration of the skin) due to inadequate oxygen circulation, severe weakness limiting even basic activities, and symptoms that persist despite treatment. The New York Heart Association (NYHA) classification system categorizes this progression from Class I (no limitation of physical activity) to Class IV (symptoms present even at rest).
Why Many People Miss the Warning Signs of Congestive Heart Failure
Heart failure symptoms often develop gradually, making them easy to attribute to aging, being out of shape, or other less serious conditions. Many people compensate for their symptoms unconsciously—they simply do less activity as fatigue increases, rarely connecting this gradual limitation to a potential heart condition. The overlap of heart failure symptoms with other conditions further complicates recognition. Shortness of breath might be dismissed as asthma or respiratory issues, while swelling could be attributed to venous insufficiency.
Psychological factors also play a role in delayed recognition. Denial is common, as people may fear acknowledging serious health problems. Some patients worry about being perceived as complainers or hypochondriacs if they mention seemingly minor symptoms like fatigue. Cultural factors can influence symptom reporting as well, with some communities less likely to seek medical care for seemingly minor issues.
Healthcare access barriers present another obstacle. Those without regular primary care may have fewer opportunities for routine screening that could detect early signs. Even during appointments, time constraints may limit thorough discussions of subtle symptoms that could signal early heart failure.
When Should You See a Doctor for Congestive Heart Failure Symptoms?
Seek immediate medical attention if you experience sudden or severe shortness of breath, chest pain, fainting, or rapid/irregular heartbeat. These could indicate a medical emergency. For less acute symptoms, make an appointment with your healthcare provider if you notice persistent fatigue that interferes with daily activities, increasing shortness of breath with activity or when lying down, or swelling in your legs, ankles, and feet that doesn’t resolve with elevation.
Other symptoms warranting medical evaluation include unexplained, rapid weight gain (more than 3 pounds in a day or 5 pounds in a week), a persistent cough, especially one that produces white or pink-tinged mucus, difficulty sleeping due to breathing problems or the need to use multiple pillows, or decreased exercise capacity compared to your normal baseline.
Those with risk factors for heart failure—including high blood pressure, coronary artery disease, diabetes, history of heart attack, or family history of heart disease—should be particularly vigilant about reporting these symptoms promptly. Regular check-ups are important even in the absence of symptoms if you have these risk factors.
Can Early Treatment Improve Outcomes for Congestive Heart Failure?
Early intervention for congestive heart failure can significantly improve long-term outcomes. Research shows that prompt diagnosis and treatment can slow disease progression, reduce hospitalizations, and extend survival. When treatment begins in earlier stages, medications tend to be more effective at controlling symptoms and preventing further heart damage. Many patients experience substantial improvement in their quality of life and functional capacity with appropriate early management.
Modern heart failure treatments target different aspects of the condition. ACE inhibitors and ARBs reduce strain on the heart, beta-blockers improve heart function over time, and newer medications like SGLT2 inhibitors have shown remarkable benefits in recent studies. Diuretics help manage fluid retention while devices like pacemakers and implantable cardioverter-defibrillators can address electrical conduction problems in appropriate patients.
Lifestyle modifications play a crucial role alongside medical therapy. Sodium restriction helps control fluid retention, while regular appropriate exercise can strengthen the cardiovascular system. Smoking cessation, limited alcohol consumption, and stress management further support heart health. Patient education about self-monitoring for symptoms and medication adherence empowers individuals to participate actively in their care.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.




