Understanding Mycosis Fungoides: A Rare Type of Skin Lymphoma
Mycosis fungoides is a rare form of cutaneous T-cell lymphoma that often begins with patchy, itchy skin and can progress over time. Learning about its early signs, diagnostic process, and available treatment options is key to managing this chronic condition effectively.

What is Mycosis Fungoides and How Does it Affect the Skin and Immune System?
Mycosis fungoides (MF) is the most common form of cutaneous T-cell lymphoma (CTCL), accounting for approximately 50-70% of all CTCL cases. It occurs when T-lymphocytes, which normally help fight infection as part of the immune system, become malignant and accumulate in the skin. These abnormal T-cells have a distinctive appearance described as cerebriform (brain-like) nuclei when examined under a microscope.
The disease affects the skin through a process where these cancerous T-cells migrate to the epidermis and form clusters called Pautrier microabscesses. This accumulation disrupts normal skin function and structure, leading to the characteristic patches, plaques, and sometimes tumors seen in affected individuals. The immune system dysfunction occurs because these malignant cells no longer perform their intended protective function, and instead contribute to chronic inflammation and potential immunosuppression as the disease progresses.
Unlike many other lymphomas, mycosis fungoides primarily stays in the skin for many years, though in advanced stages it can spread to lymph nodes, blood, and internal organs. The exact cause remains unknown, though researchers believe genetic mutations, environmental factors, and chronic antigen stimulation may play roles in its development.
Early Symptoms of Mycosis Fungoides
Mycosis fungoides typically progresses through several stages, beginning with early symptoms that can be easily mistaken for more common skin conditions. The initial presentation often includes:
-
Flat, red, scaly patches that may appear on sun-protected areas of the body such as the buttocks, lower abdomen, upper thighs, and breasts
-
Persistent itching (pruritus) that can range from mild to severe
-
Dry, flaky skin that may resemble eczema or psoriasis
-
Patches that may fade temporarily but return in the same locations
-
Areas of skin that appear lighter or darker than surrounding skin
These early symptoms may come and go for years, leading many patients to try various over-the-counter treatments without success. The patches typically grow slowly and may change in size, shape, and color over time. In some cases, patients experience what’s known as “premycotic” symptoms for up to 10 years before a definitive diagnosis is made.
As the disease progresses, patches may thicken into raised plaques with more defined borders. In more advanced stages, actual tumors may develop on the skin, and ulceration can occur. Systemic symptoms like fever, weight loss, and night sweats generally only appear in the later stages when the disease has potentially spread beyond the skin.
Common Diagnostic Tools Including Skin Biopsy and Blood Tests
Diagnosing mycosis fungoides can be challenging, often requiring multiple tests and procedures to confirm the condition. The primary diagnostic tools include:
Skin Biopsy
The gold standard for diagnosis is a skin biopsy, where a small sample of affected skin is removed and examined under a microscope. Pathologists look for characteristic features such as:
-
Epidermotropism (migration of abnormal T-cells into the epidermis)
-
Pautrier microabscesses (collections of atypical lymphocytes)
-
Band-like infiltrate of lymphocytes in the upper dermis
-
Cerebriform nuclei in the abnormal T-cells
Often, multiple biopsies from different sites may be needed, as early-stage samples may not show definitive features.
Immunophenotyping
This specialized testing identifies specific proteins on cell surfaces to determine if the T-cells are abnormal. In mycosis fungoides, the malignant cells typically express CD3 and CD4 markers while often losing CD7 and CD26 expression.
T-cell Receptor Gene Rearrangement Studies
These molecular tests look for clonal (identical) populations of T-cells, which suggest cancer rather than inflammatory conditions where T-cell populations would be diverse.
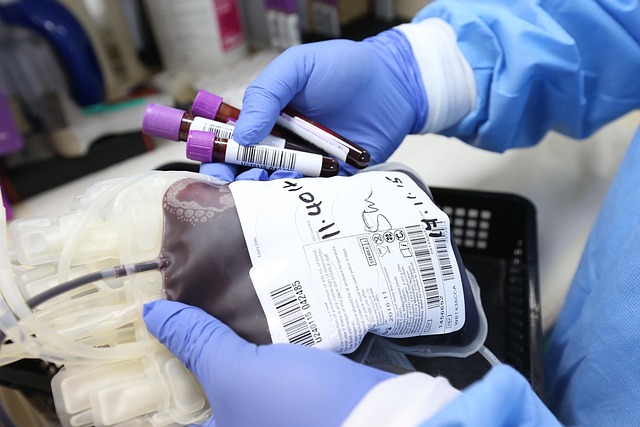
Blood Tests
Complete blood counts, flow cytometry, and Sézary cell counts can help determine if the condition has progressed beyond the skin to involve the blood (known as Sézary syndrome).
Imaging Studies
In later stages, CT scans, PET scans, or MRIs may be used to check for involvement of lymph nodes or internal organs.
The diagnostic process often involves collaboration between dermatologists, hematologists, oncologists, and dermatopathologists, sometimes requiring evaluations at specialized centers experienced with this rare condition.
Treatment Options for Mycosis Fungoides
Management of mycosis fungoides is highly individualized based on the stage of disease, overall health of the patient, and response to previous treatments. Treatment aims to control symptoms, improve quality of life, and manage disease progression rather than provide a definitive cure in most cases.
Skin-Directed Therapies
For early-stage disease limited to the skin, treatments include:
-
Topical corticosteroids to reduce inflammation and itching
-
Topical retinoids (bexarotene) that regulate cell growth
-
Topical chemotherapy agents such as mechlorethamine (nitrogen mustard)
-
Phototherapy, including narrowband UVB or PUVA (psoralen plus ultraviolet A light)
-
Local radiation therapy for resistant patches or tumors
Systemic Therapies
For more advanced disease or widespread skin involvement:
-
Retinoids (bexarotene) taken orally
-
Interferons that boost immune system function
-
Histone deacetylase inhibitors like vorinostat and romidepsin
-
Monoclonal antibodies such as mogamulizumab and brentuximab vedotin
-
Traditional chemotherapy for advanced cases
-
Extracorporeal photopheresis, where blood is treated with psoralen and UVA light
Emerging Treatments
Newer approaches include:
-
Checkpoint inhibitors that help the immune system recognize and attack cancer cells
-
CAR T-cell therapy in clinical trials
-
Allogeneic stem cell transplantation for select cases of advanced disease
Treatment costs vary widely depending on the approach, with topical therapies ranging from $100-$3,000 per month, while newer biological therapies may exceed $15,000 monthly. Most patients require long-term management with treatment adjustments over time.
| Treatment Approach | Estimated Monthly Cost | Insurance Coverage |
|---|---|---|
| Topical Corticosteroids | $50-$200 | Generally covered |
| Phototherapy (PUVA/UVB) | $1,000-$5,000 for course | Partially covered with authorization |
| Oral Bexarotene | $8,000-$12,000 | Often requires prior authorization |
| Mogamulizumab | $15,000+ | May require special approval |
| Radiation Therapy | $3,000-$10,000 per series | Typically covered for approved indications |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
Most patients with early-stage disease have an excellent prognosis with skin-directed therapies, while those with advanced disease may require more aggressive approaches. Regular follow-up with a multidisciplinary team is essential for monitoring response and adjusting treatment as needed. Patient support groups can provide valuable emotional support and practical advice for those navigating this chronic condition.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.